
The hip joint (HJ) is a complex joint made up of several bones: the femur, pubic bone, ilium, and ischium. It is surrounded by periarticular pockets and a strong muscle-ligament corset protected by subcutaneous fat and skin.
The ilium, ischium and pubic bone form the pelvic bone and are connected to the acetabulum by hyaline cartilage. These bones fuse together before the age of 16.
A distinctive feature of the femoral joint is the structure of the acetabulum, which is only partially covered with cartilage in the upper part and on the side. The middle and inferior segments are occupied by adipose tissue and the femoral ligament surrounded by a synovial membrane.
causes
Pain in the hip joint can damage intra-articular elements or adjacent structures:
- skin and subcutaneous tissue;
- muscles and ligaments;
- joint bag;
- acetabular lip (cartilaginous rim that runs along the edge of the acetabulum);
- Articular surfaces of the femur or pelvic bone.
Pain in the joint area is caused by inflammation or a violation of the integrity of its constituent structures. Most often, pain occurs when infection enters the joint cavity (infectious arthritis) and autoimmune lesion (rheumatoid and reactive arthritis).
No less common are mechanical injuries, as a result of which the epiphyses of bones, ligaments, synovial membranes and other tissues are damaged. Traumatization is more prone to active people and athletes with high physical exertion.
Elderly people who have pain in the pelvic bone due to degenerative-dystrophic cartilage changes are also at risk, as are children and adolescents in the period of hormonal changes.
Pain in the hip joint on the left or right side is caused by metabolic diseases - for example, diabetes mellitus, pseudogout and obesity.
The full list of possible diseases is as follows:
- Perthes disease;
- Arthrosis;
- Koenig's disease;
- diabetic arthropathy;
- pseudogout;
- intermittent hydration (intermittent dropsy of the joint);
- chondromatosis;
- reactive, rheumatoid and infectious arthritis;
- juvenile epiphyseolysis;
- Injury.
Perthes disease
In Perthes disease, the blood supply to the femoral head is disrupted, resulting in aseptic necrosis (death) of cartilage tissue. Children under the age of 14 mostly suffer, mostly boys.
The main symptom of Perthes disease is constant pain in the hip joint, which worsens when walking. It is not uncommon for children to complain of aching legs from the hips onwards and begin to limp.
In the early stages, symptoms are mild, leading to a late diagnosis when an indentation fracture (intra-articular fracture) already occurs. The destructive process is accompanied by an increase in pain, swelling of soft tissues and stiffness in limb movements. The patient cannot externally rotate, twist, bend, or straighten the thigh. It is also difficult to move the leg to the side.
Violations of the autonomic nervous system are also observed: the foot becomes cold and pale, while profusely sweating. Sometimes the body temperature rises to subfebrile values.
Note: In Perthes disease, the lesion can be unilateral and bilateral. In most cases, one of the joints suffers less and recovers faster.
arthrosis
Osteoarthritis of the hip joint is called coxarthrosis and is mainly diagnosed in older people. The disease progresses slowly, but causes irreversible changes. The pathological process begins with damage to the cartilage, which becomes thinner due to an increase in the density and viscosity of the synovial fluid.
The development of a coxarthrosis leads to joint deformities, muscle atrophy and a significant restriction of movement up to complete immobility. Pain syndrome in osteoarthritis has a wavy (non-permanent) character and is localized on the outer thigh, but can spread to the groin, buttocks and lower back.
In the second stage of osteoarthritis, the pain covers the inner thigh and sometimes extends to the knee. As the disease progresses, the hip pain increases and only sometimes subsides with rest.
Coxarthrosis is primary and secondary. Primary coxarthrosis develops against the background of osteochondrosis or arthrosis of the knee. Hip dysplasia, congenital hip dislocation, Perthes disease, arthritis and traumatic injuries (dislocations and fractures) can be prerequisites for secondary coxarthrosis.
Koenig's disease
If the thigh hurts laterally in the joint area, the cause may be the death of cartilage tissue (necrosis) - Koenig's disease. This condition is most common in young men aged 16 to 30 who complain of pain, limited range of motion, and periodic "pinching" of the leg.
Koenig's disease develops in several stages: first, the cartilage softens, then thickens and begins to detach from the articular surface of the bone. In the third or fourth stage, the necrotic area is shed and enters the articular cavity. This is due to accumulation of effusion (fluid), motion stiffness, and locking of the left or right joint.
Note: The presence of a "joint mouse" in the hip joint leads to the development of coxarthrosis.
diabetic arthropathy
Osteoarthropathy, or Charcot's joint, is observed in diabetes mellitus and is characterized by progressive deformity accompanied by pain of varying intensity. Painful sensations are expressed rather weakly or are completely absent, since sensitivity in this disease is sharply reduced due to pathological changes in nerve fibers.
Diabetic arthropathy occurs with a long course of diabetes and is one of its complications. It is most common in women who have not received full treatment or have been ineffective. It should be noted that the hip joints are extremely rarely affected.
pseudogout
As a result of a violation of calcium metabolism, calcium crystals begin to accumulate in the joint tissues, and chondrocalcinosis, or pseudogout, develops. The disease got its name due to the similarity of symptoms with gout, which is characterized by an attack-like course.
Acute and sharp pains appear suddenly: the affected area turns red and swells, hot to the touch. An attack of inflammation lasts from several hours to several weeks, then everything passes. With chondrocalcinosis, pain on the left or right side of the pelvis is possible.
In the vast majority of cases, pseudogout occurs without any recognizable cause and disorders of the calcium metabolism cannot be detected even during the examination. The cause of the disease is probably a local metabolic disorder within the joint. In one patient out of a hundred, chondrocalcinosis develops against the background of existing systemic diseases - diabetes, renal failure, hemochromatosis, hypothyroidism, etc.
Synovial chondromatosis
Chondromatosis of the joints, or cartilaginous islet metaplasia of the synovial membrane, mainly affects large joints, which include the hip. Most often this pathology occurs in middle-aged and elderly men, but there are cases of congenital chondromatosis.
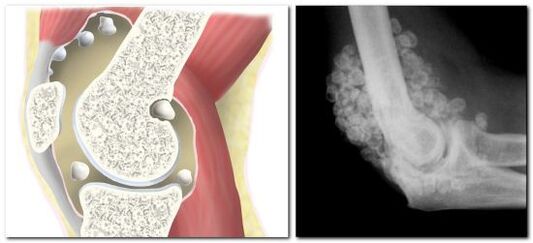
In chondromatosis, the synovial membrane degenerates into cartilage or bone tissue, as a result of which cartilage or bone bodies up to 5 cm in size are formed in the joint cavity.
The clinic of islet metaplasia is similar to arthritis: the patient is worried about pain in the hip area, leg mobility is limited, and a characteristic crunch is heard during movements.
Since chondromatosis is a dysplastic process with the formation of chondromic bodies, the occurrence of an "articular mouse" is not excluded. In this case, the "mouse" can get stuck between the articular surfaces of the bones, resulting in partial or fullBlockage of the joint leads. The joint remains blocked until the cartilaginous body enters the lumen of the capsule, and only after that movements are fully restored.
Note: Frequent or prolonged jamming of the joint can provoke the development of coxarthrosis. Complications of synovial chondromatosis include stiffness (contracture) and muscle atrophy.
arthritis
Arthritis is inflammation localized in the articular surfaces of the acetabulum and femur. The defeat of the hip joint is called coxitis, which is accompanied by dull, aching pains in the back of the thigh and groin.
There are different types of arthritis, the hip joint is most often affected by its infectious form. Other types are diagnosed much less frequently. Why does infectious arthritis occur? The development of pathology begins after bacteria and viruses enter the joint cavity.
The clinical picture of infectious arthritis can differ depending on the type of causative microorganisms. However, there are 5 characteristic signs that are observed in all patients:
- pain syndrome in the joint of the right or left leg (there is also a bilateral lesion);
- swelling and swelling over the joint;
- reddening of the skin;
- decreased motor skills;
- increase in body temperature.
At the beginning of the disease, patients feel severe pain, especially when getting up from a sitting position. The joint hurts almost constantly, because of the pain it is impossible to stand or sit. It should be noted that the infectious form of arthritis is always accompanied by fever, chills, headache, weakness and nausea.
Juvenile epiphysiolysis
The term epiphysiolysis literally means the decay, the destruction of the articular surface of the bone or the cartilage covering it. A characteristic feature of such damage is the cessation of bone growth in length, which leads to asymmetry of the lower extremities.
In adults, epiphysiolysis occurs with a fracture with displacement or rupture of the epiphysis. Destruction of the epiphysis in the growth zone is possible only in adolescence, so the disease is called juvenile.
Juvenile epiphysiolysis is an endocrine-orthopedic pathology based on an imbalance between growth hormones and sex hormones. It is these two groups of hormones that are essential for the normal functioning of cartilage tissue.
The predominance of growth hormones over sex hormones leads to a decrease in the mechanical strength of the growth zone of the femur and the epiphysis is displaced. The end portion of the bone is below and behind the acetabulum.
Typical symptoms of epiphysiolysis are pain in the right or left side of the thigh (depending on which joint is affected), lameness and an unnatural leg position. The diseased leg turns outward, the muscles of the buttocks, thighs and lower legs atrophy.
treatment
To treat Perthes disease, chondroprotectors are prescribed to promote cartilage regeneration, and angioprotectors are necessary to improve blood flow. Complex therapy also includes massage, exercise therapy, physiotherapy - UHF, electrophoresis with calcium and phosphorus, mud and ozokerite applications.
Patients with Perthes disease are recommended to offload the limb and use orthopedic devices (casts) and special beds to prevent deformity of the femoral head.
What to do with arthrosis and what drugs to drink depends on the stage of the disease. The following remedies will help relieve pain and slow down the pathological process at stages 1-2:
- nonsteroidal anti-inflammatory drugs (NSAIDs);
- vasodilators;
- muscle relaxants for relaxing muscles;
- chondroprotectors;
- hormonal (with severe pain);
- Ointments and compresses with anti-inflammatory or chondroprotective effects.
At stages 3-4, patients are shown surgery.
Koenig's disease is only treated surgically, with an arthroscopic operation the affected area of cartilage is removed.
Treatment of diabetic arthropathy includes correction of the underlying disease - diabetes mellitus, wearing special relief bandages and taking medication. All patients, regardless of the stage of the disease, are prescribed antiresorptive drugs - bisphosphonates, as well as drugs containing vitamin D and calcium. Drugs from the group of NSAIDs and corticosteroids are prescribed to relieve pain and inflammation. With infectious complications, antibiotic therapy is carried out.
There is no specific treatment for pseudogout; with exacerbations, anti-inflammatory drugs are prescribed. A large amount of fluid accumulated in the joint is indicative of an intra-articular puncture, during which the fluid is pumped out and corticosteroid medications are administered.
Chondromatosis of the hip joint requires mandatory surgical intervention, the volume of which depends on the extent of the lesion. If the number of cartilage bodies is small, they are removed by partial synovectomy (excision of the synovial membrane) or minimally invasive arthroscopy (through three punctures). The surgical treatment of a progressive form of chondromatosis can only be radical and is carried out by means of open arthrotomy or complete (total) synovectomy.
Therapy of acute infectious arthritis includes the mandatory application of a plaster cast in the area of \u200b\u200bthe hip joint, taking drugs of different groups (NSAIDs, antibiotics, steroids). With the development of a purulent process, a series of therapeutic punctures is performed to disinfect the joint.
Treatment of juvenile epiphysiolysis is surgical only. During the operation, a closed reduction of the bones is performed, for which skeletal traction is used. Then the combined parts of the bones are fixed with pins and grafts.
Absolutely all pathologies of the hip joint are serious diseases that require mandatory medical supervision. Injuries from falls or impacts that are associated with severe pain, limited mobility, and changes in joint configuration require emergency medical care. If there were no traumatic injuries and pains of varying intensity appear in the joint regularly, it is necessary to make an appointment with a family doctor or rheumatologist and undergo an examination.






























